Transpulmonary Pressure: Time to individualize the ventilator.
- Michael Ritchie
- May 15, 2021
- 6 min read
Spending time to optimize the patient on the pressure curve will pay dividends in the long run. It will improve patient synchrony which could potentially lead to quicker extubations. When trying to optimize someone on the ventilator, it is important to understand alveolar physiology and the pressure-volume loop. The alveoli are coated in surfactant, which helps alveoli work efficiently. It reduces the surface tension of the alveoli. The surface tension wants to collapse the alveoli and competes with the expanding force of the gas. Laplace’s law looks at the pressure needed to keep an equilibrium at the alveolar level.
Laplace’s Law: P = 2γ/r
Pressure (P), surface tension (γ), radius (r)
Surfactant prevents atelectasis, improves compliance, and helps recruit other alveoli. The alveoli are often described as balloons. When a balloon is uninflated they are difficult to expand, then they reach a critical opening pressure and it becomes much easier. Surfactant helps the alveoli stay in a partially open, easily expandable, state. It is this expanded state that is important to pulmonary compliance.
TPP can be looked at in inspiration or expiration, but for this discussion, the focus will be during expiration. Transpulmonary pressure (TPP) is the pressure needed to keep the alveoli distended.
Transpulmonary pressure = Alveolar pressure (Palv) – Pleural pressure (Ppl)
There are opposing forces at the pleural interface. The lung wants to collapse and the ribs want to expand out. The pleural pressure is the pressure from the ribs being under stress and wanting to expand. This is why the pleural pressure is negative. If the alveolar pressure was 0, and the pleural pressure is usually -4, this means the transpulmonary pressure is 4
Transpulmonary pressure = Palv (0) – Ppl (-4)
TPP = 0 - - 4
TPP = 0 + 4
TPP = 4
The goal is to have a positive transpulmonary pressure, this is what keeps the alveoli open. Looking at the pressure-volume loop, a positive transpulmonary pressure would keep the lungs above the lower inflection point. The lower inflection point (LIP) is the pressure needed to recruit all the alveoli possible. When all possible alveoli are recruited without over distending the alveoli, it gives the greatest surface area for expansion. This means more change in volume for a given change in pressure, which is increased compliance.
Compliance = △V/△P
Figure 1: Pressure-Volume Curve
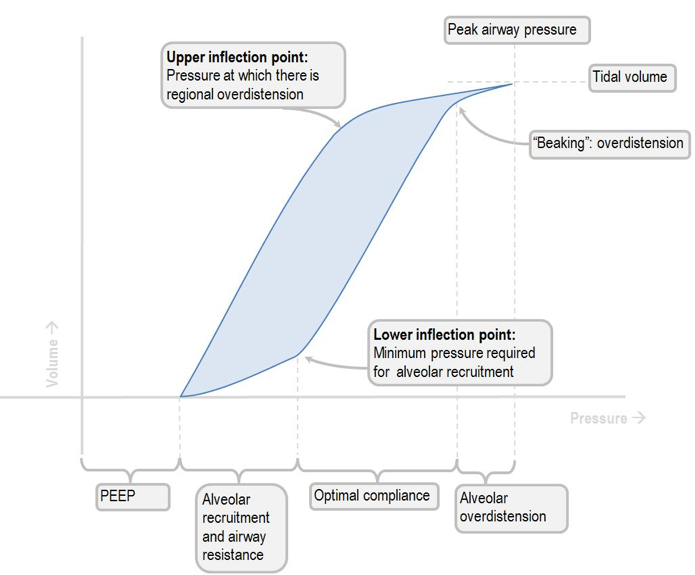
The two main things I focus on then approaching the ventilator are getting above the lower inflection point (LIP) and optimizing driving pressure. Driving pressure, as mentioned in a previous blog, is Volume/Static Compliance. The better the compliance, the lower the driving pressure. By spending time getting above the LIP you can optimize compliance, reduce driving pressure, and improve patient outcomes.
How do you get above the lower inflection point?
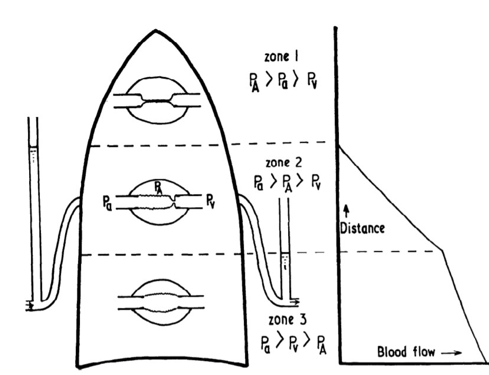
The key is the transpulmonary pressure. The TPP is actually in opposition to the chest wall pressure, but it is not often described this way. As mentioned above, the TPP is positive and keeps the lungs expanded at rest. The chest wall pressure is minimal in many patients, but in a certain population of patients, the chest wall/abdominal pressure can make a profound impact on the TPP.
I write the transpulmonary pressure to include the chest wall pressure. This helps me visually in understanding the forces leading to atelectasis and poor lung compliance.
My modified equation: TPP = Palv – (Ppl + Pcw)
Chest wall pressure (Pcw) includes the abdomen and pressure exerted on the diaphragm. It is any pressure that is putting an inward force on the lungs.
Example: Two Patients intubated with a PEEP =5

In the example above, due to increased chest wall pressure in patient 2, there is a negative transpulmonary pressure. This leads to lung collapse and atelectasis. Atelectasis decreases compliance and leads to higher ventilator settings. If the PEEP is increased for patient 2 to a PEEP of 20 cmH20, then they will have a positive TPP, be above the LIP and have better compliance and lower ventilator settings.
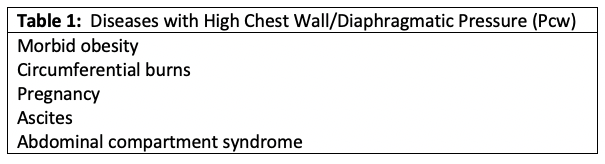
Other signs that the patient has a negative TPP can be seen on x-ray. Based on the West zones, which look at the relationship of alveolar, arterial, and venous pressure, the most common area for collapse is zone 3.
Figure 2: West Zones
https://derangedphysiology.com/main/cicm-primary-exam/required-reading/respiratory-system/Chapter%20072/wests-zones-lung
In zone 3, the arterial and venous pressure are higher than the alveolar pressure. This leads to alveolar collapse and atelectasis. Atelectasis means there is perfusion without ventilation which is a shunt. When a patient has a negative TPP they will have low lung volumes and an x-ray that reads bilateral lower lobe atelectasis.
If you find your obese patients on high vent settings (i.e. high driving pressure, low compliance, high fiO2 requirements), it may be due to under PEEPing patients. Do not be afraid to increase PEEP in a patient you suspect has high chest wall pressure. The PEEP needed to overcome the chest wall pressure can be >30 cmH20 in some patients.
How do you know what the chest wall pressure is so you can find the ideal PEEP?
There are a number of ways to get close to the correct answer. There are probably too many variables for one way to be completely accurate. The two main methods are testing different PEEPs until the best compliance is found and measuring a surrogate for chest wall pressure.
Method #1:
Pressure/Volume Loop:
The PEEP can be adjusted in small increments and the change in compliance can be measured. As the PEEP goes above the lower inflection point the compliance improves until its increase leads to overexpansion and the compliance decreases again. This method can be done manually and the PEEP increased in increments and allowed to recruit and the new compliance measured. A quicker method is through the ventilator and many ventilators now do this for you. The ventilator will slowly increase the pressure, measure the compliance, and map out a pressure-volume curve. This will show the lower and upper inflection points and help set the ideal PEEP.
Method #2:
Esophageal balloon
Esophageal pressure has been found to be a good surrogate for the external pressure exerted on the lungs. By inserted an esophageal balloon the pressure across the esophagus can be measured. This pressure is used for the chest wall pressure. The PEEP is typically set to this pressure.
Figure 3: Esophageal Balloon Placement

Piraino T, Cook D. Optimal PEEP Guided by Esophageal Balloon Manometry. Respir Care 2011;56:510 –513
The waveform of the esophageal pressure should show the heartbeat and can be shown on the ventilator.
Figure 4: Ventilator Scalars with Esophageal Balloon

Hess D. Respiratory Mechanics in Mechanically Ventilated Patients. Respir Care 2014;59:1773-1794
In the example in Figure 4, the esophageal pressure was found to be 26 cmH20 and the PEEP was set to the esophageal pressure. This improved the compliance and the driving pressure was only 14 cmH20 post intervention.
Complications after intubation:
Obese patients are a common example of patients who decompensate after intubation. These patients are often able to compensate/auto-peep themselves when they are awake and breathing on their own. It seems they are able to generate auto-peep by partially closing their glottis and then able to overcome the chest wall pressure. This is lost when they are intubated and the endotracheal tube inserted and leads to derecruitment after intubation if their intrinsic PEEP is not maintained.
If you are seeing obese patients decompensating frequently after intubation, consider that they are under-PEEPed.
The obese patient requiring tracheostomy:
The obese patient population is also unique after requiring a tracheostomy. When they are trached and placed on a trach collar or T-piece, they lose the PEEP from the ventilator and can derecruit. This leads to prolonged ventilator weans on these patients. Studies have shown that taking these patients from the vent straight to a Passy-Muir valve led to shorter ventilator weans because it allowed them to start generating their own PEEP (5).
I think using the modified TPP equation makes it easier to understand and visualize what is happening to the patient. By identifying patients at high risk for high chest wall pressure, you can make a big difference in how they tolerate the vent.
Putting it all together:
Transpulmonary pressure during inspiration also has its uses, but for this, we are focusing on TPP during expiration. If we look at the modified TPP equation and equate the chest wall pressure to weight sitting on the alveoli, it should make it easier to visualize how matching the PEEP with the chest wall pressure will keep the alveoli expanded. So do not be afraid of PEEP, some patients just need more and it is time to individualize.
Modified TPP = Palv – (Ppl + Pcw)
= PEEP – (Ppl + Pcw)
= PEEP – Pcw
Figure 5: Negative Transpulmonary Pressure
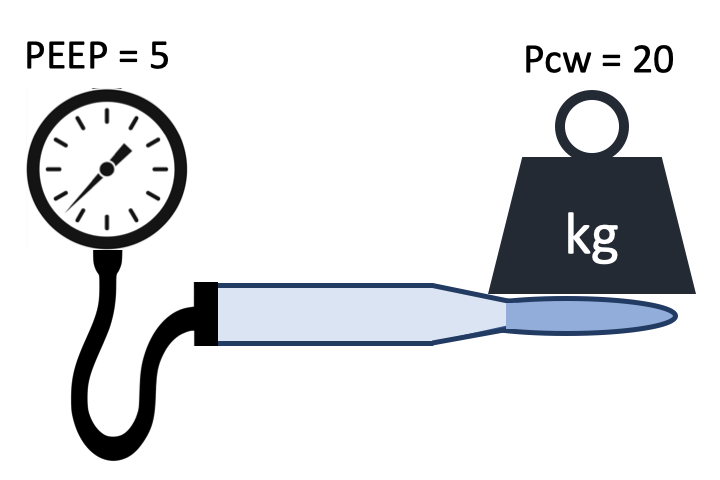
Figure 6: Positive Transpulmonary Pressure

References:
1. Harris RS. Pressure-volume curves of the respiratory system. Respir Care. 2005;50(1):78-99.
2. Neupane K, Jamil RT. Physiology, Transpulmonary Pressure. [Updated 2020 Jun 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www-ncbi-nlm-nih-gov/books/NBK559004/
3. Piraino T, Cook DJ. Optimal PEEP guided by esophageal balloon manometry. Respir Care. 2011;56(4):510-513. doi:10.4187/respcare.00815
4. Hess DR. Respiratory mechanics in mechanically ventilated patients. Respir Care. 2014;59(11):1773-1794. doi:10.4187/respcare.03410
5. Obi ON, Mazer M, Bangley C, et al. Obesity and Weaning from Mechanical Ventilation-An Exploratory Study. Clin Med Insights Circ Respir Pulm Med. 2018;12:1179548418801004. Published 2018 Sep 18. doi:10.1177/1179548418801004






Comments