A Test in Respiratory Physiology
- Michael Ritchie
- Apr 5, 2021
- 4 min read
A new patient just arrived in the ICU who was intubated for altered mental status. The emergency department reported concerns for opiate overdose leading to the altered mental status.
An arterial blood gas was done upon arrival to the ICU:
pH: 7.05 paO2: 146 pCO2: 97 HCO3: 26 Base Excess: -5.7
The patient’s current ventilator settings are PRVC: TV 500mL; RR: 10bpm; FiO2: 50%; PEEP 5cmH20

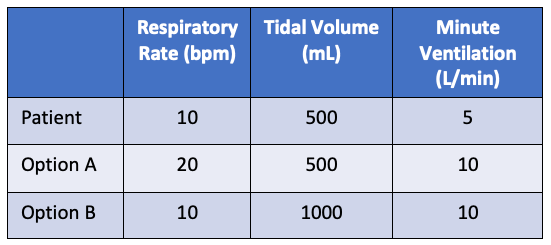
You want to bring down their CO2 as quickly and efficiently as possible. You know that increasing ventilation will decrease their CO2. For this exercise, you have a choice of doubling the respiratory rate (RR) to 20bpm (Option A) or doubling the tidal volume (TV) to 1000mL (Option B).
Let’s assume that the patient will tolerate either change with no breath stacking, ventilator induced lung injury, or any other negative side effects.
Which one will lower the CO2 most efficiently?
A. Doubling the RR
B. Doubling the TV
C. They are equal
Answer:
There is no gas exchange in the trachea, bronchi, or terminal bronchioles. Since there is no gas exchange, this is dead space, or more specifically this is the anatomical dead space. There is only gas exchange in the respiratory zone. The respiratory zone is made of respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli.
The actual ventilation is ventilation in the respiratory zone or the alveolar minute ventilation. Alveolar minute ventilation is defined as the minute ventilation minus the anatomical dead space. The amount of anatomical dead space varies between people depending on their height. The estimated amount is 30% of the tidal volume. For a patient with an average TV of 500mL, the anatomical dead space would be 150mL.
Relooking at the problem and focusing on alveolar minute ventilation, a more accurate representation of actual gas exchange for this patient is observed.
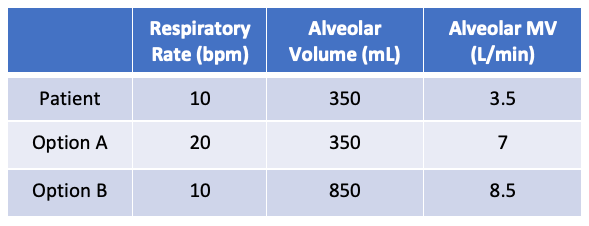
It is now easy to see that the answer is B: doubling the tidal volume.
Definitions:
Tidal Volume: The amount of air that moves in and out of the lungs per respiratory cycle
Anatomical dead space: The portion of the airway that does not participate in gas exchange
Alveolar volume: The portion of the airway that is able to participate in gas exchange.
Alveolar dead space: The volume of the alveoli that do not participate in gas exchange.
Negligible in healthy lungs
Physiological dead space: Anatomical dead space + alveolar dead space.
Dead space ventilation: Physiological dead space X respiratory rate
Total ventilation (minute ventilation): Tidal volume X respiratory rate
Alveolar ventilation (alveolar minute ventilation): Alveolar volume X respiratory rate
Alveolar Minute Ventilation:
Looking at a patient’s ventilation in terms of alveolar minute ventilation is a more specific way of looking at patient’s actual minute ventilation. It means increasing tidal volume is a more efficient way of increasing minute ventilation. The actual answer is obviously more complex. Increasing the TV can lead to worsening ventilator lung injury with volutrauma and barotrauma. Looking at the other side of minute ventilation, increasing RR can limit expiratory time and can lead to breath stacking and auto-peeping.
The other type of dead space is alveolar dead space. Alveolar dead space is the volume that gets to the alveoli but is not able to participate in gas exchange. This happens in certain disease states where damage compromises a portion of the alveoli. The amount of alveolar dead space depends on the extent of the disease state.
Physiologic dead space is the addition of anatomical and alveolar dead space. Physiologic dead space is the total dead space per breath, making dead space ventilation the physiologic dead space multiplied by RR.
For example, COPD patients have damage to the lung parenchyma and increased dead space. For a COPD patient, giving at 500mL tidal volume may only be 250mL of alveolar volume after accounting for damage, meaning 500mL would be under-supporting the patient leading to ventilator dyssynchrony.
COPD patients prefer a long deep breath with a long expiratory time. This is to overcome the increased dead space and the increased resistance to expiration. People will often decrease the patient’s inspiratory time to increase expiratory time. But, decreasing inspiratory time can make the patient more dyssynchronous. They need a long deep breath as much as a long expiratory time.
Calculating physiological dead space:
Knowing the patient’s physiological dead space can help optimize the patient to ensure appropriate ventilation. While anatomical dead space will not change depending on the patient’s critical illness, the alveolar dead space can change. The amount of dead space can be calculated using the modified Bohr’s equation (Enghoff’s equation).
Enghoff’s equation: Vd = ((PaCO2 - PeCO2)/PaCO2) X TV
Vd: Dead space ventilation
PaCO2: Partial pressure of arterial CO2
PeCO2: Partial pressure of expired CO2
TV: Tidal volume
PeCO2 can be obtained by placing an end-tidal CO2 monitor in-line with the ventilator.

https://johnsonfrancis.org/professional/etco2-monitoring-in-icu-capnography/
Example:
Values: PaCO2: 40mmHg, PeCO2: 28mmHg, TV: 500mL
Vd = ((40mmHg-28mmHg)/40mmHg)x500mL
Vd = 150mL
This is 30% of the total TV, which means there is probably very little alveolar dead space.
This equation can be used to adjust the ventilator in intubated critically ill patients. Optimizing tidal volume and lowering respiratory rate will help with increasing alveolar minute ventilation with the minimizing ventilator settings.
In the non-intubated patient, the nose, mouth, nasopharynx, oropharynx, and hypopharynx also contribute to anatomical dead space. This helps with explaining how high-flow nasal cannula helps reduce CO2 by decreasing anatomical dead space. With the higher flow rates, the high-flow nasal cannula will wash away the CO2 in the nose, mouth, nasopharynx, oropharynx, and hypopharynx which will create a slightly lower anatomical dead space volume.
Hopefully this helps with better understanding ventilation to help with optimizing the patient and reducing ventilator dyssynchrony and improving patient comfort and compliance on the ventilator.
References:
1. Quinn M, St. Lucia K, Rizzo A. Anatomy, Anatomic Dead Space. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan.
2. Intagliata S, Rizzo A, Gossman WG. Physiology, Lung Dead Space. [Updated 2020 Sep 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan
3. Kiiski R, Takala J, Eissa NT. Measurement of alveolar ventilation and changes in deadspace by indirect calorimetry during mechanical ventilation: a laboratory and clinical validation. Crit Care Med. 1991 Oct;19(10):1303-9.






Great entry. I like the 1000 mL tidal volume. Assuming his predicted body weight is 166.67 kg then he must be 11 feet 10 inches tall.